Snowcamp-SBT
We are delighted to be working alongside Snow-Camp Charity offering mental health support to 13-21 year olds.
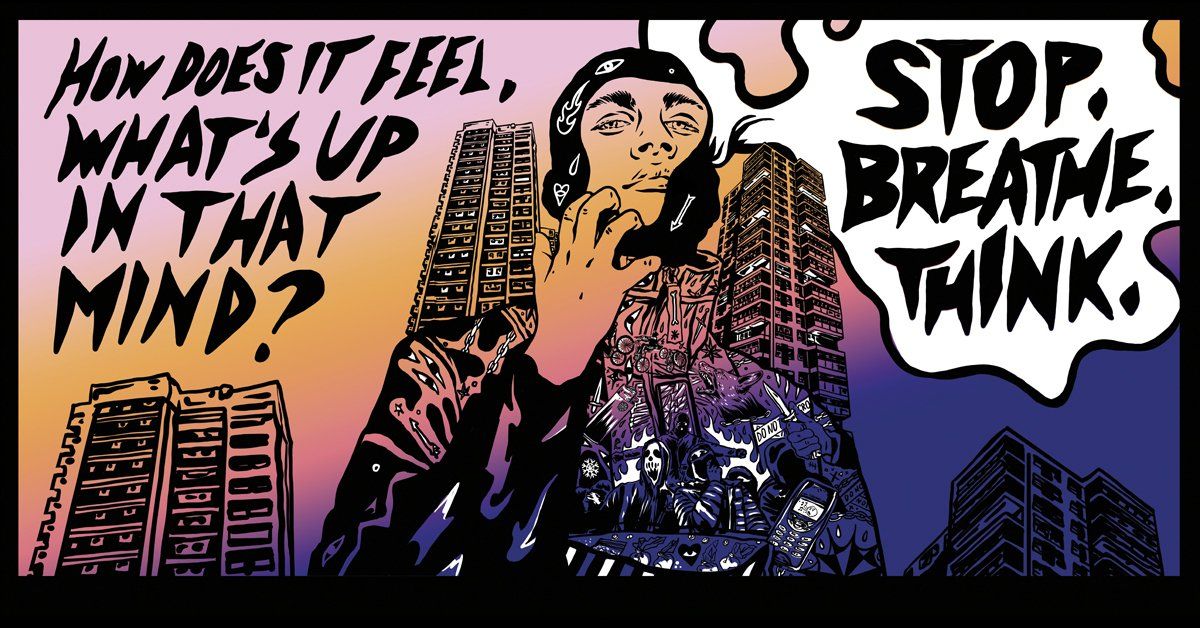
Snow-Camp has launched Stop.Breathe.Think, a mindfulness campaign using drill music to help tackle knife crime.
Stop.Breathe.Think
brings together drill artists and mindfulness experts to provide mindfulness techniques to help young people manage their emotions. The campaign will also encourage young people across the UK to sign up for the charity’s free series of mindfulness tutorials and free 1-1-counselling sessions.
Mindfulness, the ability to be fully present in the moment, teaches us how to change a rash, reactive mindset into a more considered, responsive and productive one. It provides practical ways to become less reactive, and more able to manage impulsive feelings and behaviours. Although mindfulness doesn’t eliminate factors that may lead to knife crime, such as fear, anger and anxiety, the charity hopes that by providing young people with mindfulness techniques, they can become better equipped to handle their emotions in the moment – with a better chance of reacting calmly.
Nito NB, an up and coming artist from West London, has created the campaign’s first drill track titled Breathe, that teaches young people how to use mindfulness to deal with anger. Whilst growing up, Nito’s mum became his coping mechanism, she taught him how to channel and process his anger. Through his track, Breathe, Nito hopes to raise awareness of the usefulness of mindfulness techniques and the importance of being aware of your emotions. Although drill music has been accused of encouraging knife crime, the charity wants to use a relatable and authentic vehicle to reach as many young people as possible.
Over recent months, whilst delivering its own mental health programme, Snow-Camp has seen that mental wellbeing is something that today’s young people are increasingly struggling with, which has been exacerbated by COVID-19. Young people rarely have the means or resources to find the support they need. Ninety-two percent of young people on Snow-Camp’s programme believe that the rise in knife crime is linked to young people’s mental health issues and challenges related to controlling emotions. That’s why Stop.Breathe.Think is also offering young people across the UK the opportunity to sign up for the charity’s free series of mindfulness tutorials and free 1-1-counselling sessions.
Nito NB’s track will be hosted on LinkUp TV, whilst promotion through posters and billboards in key inner-city locations aims to enable the campaign to reach further young people. Young people can sign-up for the free mindfulness tutorials and 1-1-counselling sessions via the Stop.Breathe.Think website.

Obsessive-Compulsive Disorder, or OCD , is a mental health condition that is often misunderstood. It's more than just being "a little neat" or "a bit of a clean freak." For those who live with it, OCD is a debilitating cycle of unwanted thoughts and repetitive behaviours that can seriously disrupt daily life. Understanding this cycle is the first step toward reclaiming control. What Exactly is OCD? OCD is defined by a pattern that has two main parts: obsessions and compulsions . 1. Obsessions These are unwanted, intrusive, and distressing thoughts, images, or urges that repeatedly enter your mind. They cause intense anxiety, fear, or disgust. Common obsessions include: Contamination fears (e.g., fear of germs, dirt, or illness). Harm obsessions (e.g., fear of accidentally or deliberately hurting yourself or others). A need for symmetry, order, or "just-right" feelings. Unwanted aggressive, sexual, or religious thoughts (sometimes called scrupulosity). It is crucial to remember that these thoughts are ego-dystonic —they go against the person's true values, character, and intentions. They are thoughts, not facts. 2. Compulsions These are repetitive behaviours or mental acts that a person feels driven to perform in response to the obsession. The goal of a compulsion is to temporarily reduce the anxiety caused by the obsession or to prevent a feared event from happening. Common compulsions include: Excessive cleaning and hand-washing. Repeatedly checking locks, appliances, or safety measures. Ordering and arranging objects in a precise way. Mental rituals like counting, repeating phrases, or 'neutralizing' a bad thought. Excessively seeking reassurance from others. The cycle looks like this: Obsession → Anxiety → Compulsion → Temporary Relief → Obsession Returns. The compulsion only reinforces the idea that the obsession was a real threat that needed to be addressed. What Helps with OCD Management? If you are struggling with OCD, help is available. While it can feel overwhelming, evidence-based treatments and self-help strategies can significantly improve your quality of life. The Gold Standard Treatment The most effective, evidence-based treatment for OCD is a form of Cognitive Behavioural Therapy (CBT) called Exposure and Response Prevention (ERP) . Exposure (E): This involves gradually and repeatedly confronting the thoughts, images, objects, or situations that cause your obsessions and anxiety. Response Prevention (RP): This means choosing to resist the urge to perform the compulsion or ritual that usually follows the exposure. For example, a person with contamination fears might be asked to lightly touch a doorknob (exposure) and then be guided by the therapist to not wash their hands for a set amount of time (response prevention). Over time and with practice, the anxiety naturally decreases, and the brain learns that the feared consequence does not occur, thus breaking the cycle. This should always be done with a therapist trained in ERP. In some cases, Selective Serotonin Reuptake Inhibitors (SSRIs) , a type of antidepressant medication, may be prescribed by a doctor to help reduce anxiety and allow the person to engage more effectively in therapy. Often, a combination of ERP and medication is the most effective approach. Practical Self-Help Strategies While professional treatment is essential, there are daily self-help strategies that can support your recovery: 1. Accept the Thoughts, Resist the Response Practice 'Un-Fusing' from Thoughts: Recognise an obsessive thought as simply a thought, not a command or a reflection of reality. You can say to yourself, "That's just my OCD thought about germs," instead of engaging with the thought's content. Embrace Uncertainty: OCD thrives on the need for 100% certainty. You can counter this by intentionally introducing and accepting small amounts of doubt. Use phrases like, "Maybe that's true, maybe it isn't. I'm going to choose to move on anyway." Delay the Compulsion: If resisting a compulsion entirely feels impossible, try delaying it. Say, "I will do this in 5 minutes," and gradually increase the delay time. 2. Build Healthy Habits Mindfulness: Practising mindfulness helps you focus on the present moment without judgement. This can reduce the tendency to get carried away by anxious thoughts about the past or future. Sleep and Nutrition: Ensure you are getting adequate sleep and a balanced diet. Fatigue and low blood sugar can exacerbate stress and anxiety, making OCD symptoms feel worse. Movement: Regular physical activity is a powerful stress reducer and can help regulate mood and anxiety levels. 3. Cultivate Support Connect with Trusted People: OCD is isolating. Talk about your struggles with a trusted friend, family member, or join an OCD support group . Sharing your experience can reduce feelings of shame and isolation. Avoid Excessive Reassurance Seeking: While reassurance provides temporary relief, it is a form of compulsion and strengthens the OCD cycle. Gently ask loved ones to stop giving reassurance and instead offer distraction or emotional support. If you believe you or a loved one may be affected by OCD, the most important step is to speak with a healthcare professional or a specialist who can provide a diagnosis and guide you to a qualified ERP therapist. You don't have to face this alone.
Understanding Your Diagnosis Receiving an ADHD diagnosis as an adult can be a mix of relief and uncertainty. It might finally explain the challenges you've faced, but it also raises new questions. Here’s how to cope with this significant life event: 1. Educate Yourself Research ADHD: Learn about the symptoms, causes, and treatment options. This knowledge can empower you to manage your condition effectively. Join Support Groups: Connect with others who understand what you're going through. Sharing experiences can be incredibly helpful. 2. Accept and Embrace Your Diagnosis Avoid Self-Blame: ADHD is a neurodevelopmental disorder, not a personal failing. Celebrate Your Strengths: Focus on your unique talents and abilities, which can often be enhanced with the right strategies. 3. Develop Coping Mechanisms Mindfulness and Meditation: These practices can help manage stress and improve focus. Exercise: Regular physical activity can boost mood, energy, and cognitive function. Healthy Lifestyle: Prioritize a balanced diet, sufficient sleep, and stress management techniques. 4. Build a Support Network Lean on Loved Ones: Share your feelings with trusted friends and family. Seek Professional Help: A therapist can provide guidance, coping strategies, and support. 5. Explore Treatment Options Medication: Discuss medication options with your doctor. It can be a valuable tool for managing symptoms. Therapy: Cognitive-behavioral therapy (CBT) can help develop effective coping skills and strategies. Lifestyle Adjustments: Explore accommodations and strategies to help you succeed at work, school, and home. 6. Give Yourself Time Be Patient: Adjusting to a new diagnosis takes time. Be kind to yourself as you learn to navigate your experiences. Celebrate Progress: Acknowledge your achievements, no matter how small. Remember, you're not alone. Many adults with ADHD lead fulfilling lives. With the right support and strategies, you can thrive and overcome challenges. Why not schedule a consultation with JHD Counselling to see how we may be able to steer you in the right direction
National Coming Out Day is a time for LGBTQ+ individuals to celebrate their identities and live authentically. However, coming out can also be a challenging experience, especially when faced with negative reactions from family and friends. If you're experiencing fallout from coming out, know that you're not alone. Many LGBTQ+ individuals face similar challenges. Here are some tips to help you cope: 1. Prioritise Your Mental Health Seek support: Reach out to friends, family members, or a therapist who is supportive of your identity. Practice self-care: Engage in activities that help you relax and de-stress, such as meditation, exercise, or spending time in nature. Join a support group: Connecting with others who have gone through similar experiences can provide valuable support and understanding. 2. Set Boundaries Communicate your needs: Clearly express your boundaries to those who are struggling to accept your identity. Limit contact: If necessary, limit your contact with individuals who are causing you significant distress. 3. Build a Support Network Connect with the LGBTQ+ community: Join local LGBTQ+ organizations or online communities to find support and a sense of belonging. Reach out to friends and family who are supportive: Spend time with people who accept and love you for who you are. 4. Focus on Your Well-being Remember your worth: Your identity is valid and valuable, regardless of others' opinions. Celebrate your journey: Acknowledge the courage it takes to come out and celebrate your progress. At JHD/CHD, our founder, Carol, is a proud member of the LGBTQ+ community. We understand firsthand the challenges that can arise when coming out. Our team of experienced counselors is dedicated to providing compassionate and supportive care to individuals who are navigating their identities. If you're struggling to cope with fallout from coming out, please don't hesitate to reach out to us. We're here to help you through this potentially difficult time.
